TCT 2025: ShortCUT Trial Compares Cutting Balloon Angioplasty and Intravascular Lithotripsy (IVL) for Calcified Coronary Artery Disease
- byDoctor News Daily Team
- 28 October, 2025
- 0 Comments
- 0 Mins
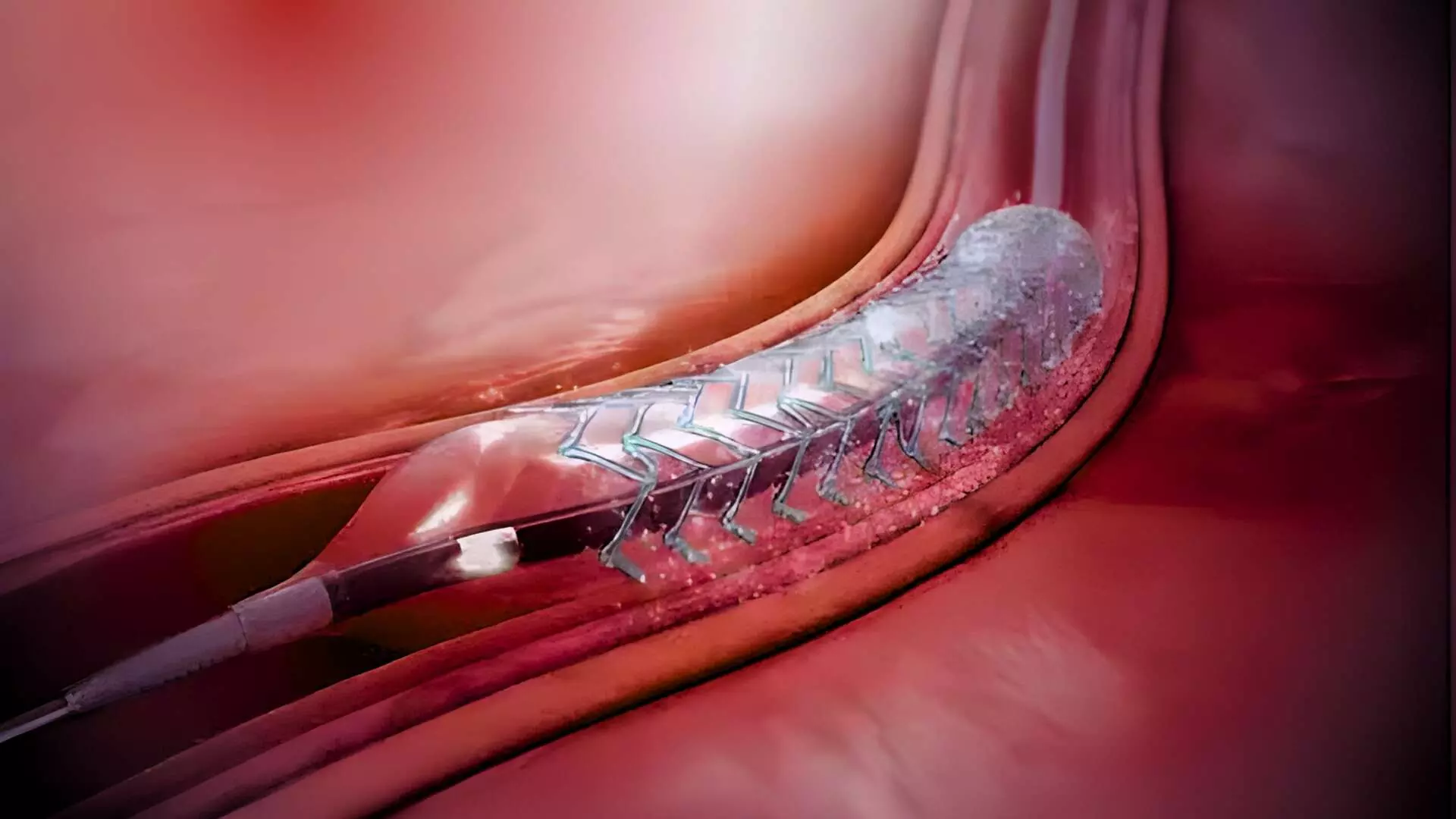
This news is covered by the Bureau present at the TCT Conference 2025, being held in San Francisco, USA. Cutting balloon angioplasty was found to be non-inferior to intravascular lithotripsy (IVL) in achieving optimal stent expansion for patients with moderate-to-severely calcified coronary lesions undergoing percutaneous coronary intervention (PCI), according to results of the ShortCUT trial presented by Dr. Suzanne J. Baron at TCT 2025. The study also found that cutting balloon angioplasty offered similar procedural and clinical outcomes at a significantly lower procedural cost. The ShortCUT trial is the first adequately powered, randomized controlled trial to compare intravascular lithotripsy to other balloon-based device for the treatment of calcified coronary artery disease. The trial enrolled 413 patients at 21 U.S. sites, including those presenting with stable angina or non-ST elevation acute coronary syndromes (NSTE-ACS) and moderate-to-severe coronary calcification confirmed by intravascular ultrasound (IVUS). Patients with STEMI, cardiogenic shock, or excessive vessel tortuosity were excluded. Participants were randomized 1:1 to receive either IVL or cutting balloon angioplasty, with or without planned rotational atherectomy, prior to drug-eluting stent (DES) implantation. The primary endpoint was post-procedural minimal stent area (MSA) at the site of maximal calcium burden, as adjudicated by an independent IVUS core laboratory. Across the entire study population, the mean post-procedural MSA was 8.6 ± 2.5 mm² with IVL and 8.0 ± 2.4 mm² with the cutting balloon. The between-group difference of 0.6 mm² met the prespecified criterion for non-inferiority (p=0.007). There was no statistical difference in superiority testing (p=0.993). Stent expansion, calcium fracture rates, and strategy success—defined as stent delivery with residual stenosis <20% without requiring an alternative device, were similar between groups (89.7% for IVL vs. 89.2% for cutting balloon). In subgroup analyses, findings were consistent among patients undergoing planned rotational atherectomy. In those without planned atherectomy, IVL achieved a slightly larger MSA (8.8 ± 2.7 mm² vs. 7.7 ± 2.3 mm²), though both approaches resulted in high rates of stent expansion and similar calcium fracture patterns. Cutting balloon angioplasty did not meet non-inferiority, however this may have been partly due to differences in vessel size between groups, as stent expansion and indices of fracture were similar. Safety outcomes were excellent, with low complication rates in both groups. The incidence of intraprocedural adverse events and 30-day major adverse cardiac and cerebrovascular events (MACCE) was identical at 2.9%. Device-related complications such as perforation, abrupt closure, or significant dissection were infrequent and comparable. However, a notable finding was the substantial cost difference between the two modalities. The mean total procedural cost per target vessel was $13,051 for IVL compared with $9,409 for cutting balloon angioplasty, representing a cost difference of $3,632 (p<0.001). This cost gap was consistent across both planned and non-planned atherectomy cohorts. Investigators concluded that cutting balloon angioplasty is a reasonable, cost-effective, and widely accessible alternative to IVL for the treatment of significantly calcified coronary lesions when guided by intravascular imaging. While both techniques achieved similar safety and efficacy, the lower procedural cost of the cutting balloon approach could have important implications for practice, especially in cost-sensitive healthcare settings. Reference:Suzanne J. Baron et al., The ShortCUT Trial: Shockwave Lithotripsy Compared to Cutting Balloon Treatment in Calcified Coronary Artery Disease, TCT Conference 2025, San Francisco.https://www.tctconference.com/
Disclaimer: This website is designed for healthcare professionals and serves solely for informational purposes.
The content provided should not be interpreted as medical advice, diagnosis, treatment recommendations, prescriptions, or endorsements of specific medical practices. It is not a replacement for professional medical consultation or the expertise of a licensed healthcare provider.
Given the ever-evolving nature of medical science, we strive to keep our information accurate and up to date. However, we do not guarantee the completeness or accuracy of the content.
If you come across any inconsistencies, please reach out to us at
admin@doctornewsdaily.com.
We do not support or endorse medical opinions, treatments, or recommendations that contradict the advice of qualified healthcare professionals.
By using this website, you agree to our
Terms of Use,
Privacy Policy, and
Advertisement Policy.
For further details, please review our
Full Disclaimer.
Recent News
PG AYUSH: DME Gujarat notifies schedule for Round...
- 28 October, 2025
Delhi Doctor accused under PCPNDT Act gets court r...
- 28 October, 2025
TCT 2025: ShortCUT Trial Compares Cutting Balloon...
- 28 October, 2025
Daily Newsletter
Get all the top stories from Blogs to keep track.


0 Comments
Post a comment
No comments yet. Be the first to comment!