Carvedilol Improves Survival In Cirrhosis Patients: Study
- byDoctor News Daily Team
- 02 July, 2025
- 0 Comments
- 0 Mins
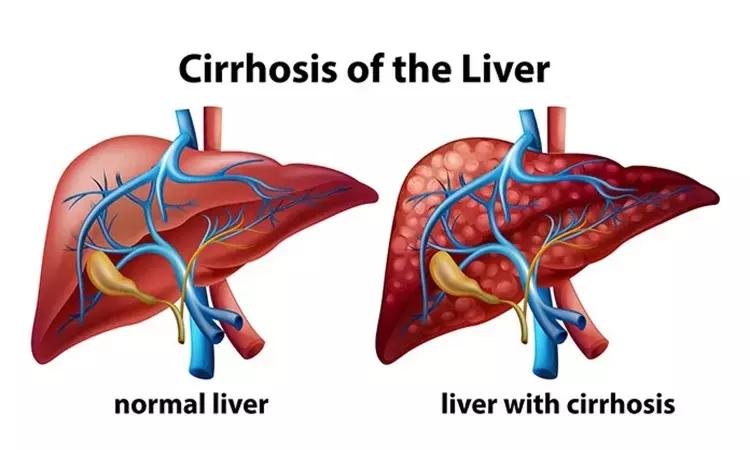
UK: The use of carvedilol improves overall survival in patients with cirrhosis and portal hypertension, finds a recent study in the journal Alimentary Pharmacology & Therapeutics.
In patients with cirrhosis with portal hypertension, primary prophylaxis of variceal haemorrhage with non‐selective beta blockers (NSBB) or variceal band ligation (VBL) is the standard of care. NSBB, and particularly carvedilol may improve survival. Hannah R. McDowell, Department of Hepatology, Royal Infirmary of Edinburgh, Edinburgh, UK, and colleagues aimed to assess mortality in a cohort of patients previously randomised to either carvedilol or VBL.
For the purpose, the researchers retrospectively analysed 152 patients who were recruited to a multi‐centre randomised controlled trial between 7 April 2000 and 24 June 2006. The trial was designed to assess the efficacy of VBL versus carvedilol in preventing first variceal bleed.
The researchers used electronic records to undertake long‐term follow‐up (up to 20 years). The primary outcome of all‐cause mortality and secondary end points of liver‐related mortality and decompensation events (ascites, encephalopathy, variceal bleeding).
152 patients were included in analysis with baseline characteristics well matched between the carvedilol (n = 77) and VBL (n = 75) groups.
Key findings of the study include:
In the intention‐to‐treat analysis, carvedilol offered a significant survival advantage with median survival of 7.8 years compared to 4.2 years in the VBL group.
This survival benefit was maintained in per‐protocol analysis when patients who crossed between treatment arms were excluded.
Transplant‐free survival, liver‐related mortality and decompensation events were similar in both groups.
The study titled, "Carvedilol is associated with improved survival in patients with cirrhosis: a long‐term follow‐up study," is published in the journal Alimentary Pharmacology & Therapeutics.
DOI: https://onlinelibrary.wiley.com/doi/abs/10.1111/apt.16189
Disclaimer: This website is designed for healthcare professionals and serves solely for informational purposes.
The content provided should not be interpreted as medical advice, diagnosis, treatment recommendations, prescriptions, or endorsements of specific medical practices. It is not a replacement for professional medical consultation or the expertise of a licensed healthcare provider.
Given the ever-evolving nature of medical science, we strive to keep our information accurate and up to date. However, we do not guarantee the completeness or accuracy of the content.
If you come across any inconsistencies, please reach out to us at
admin@doctornewsdaily.com.
We do not support or endorse medical opinions, treatments, or recommendations that contradict the advice of qualified healthcare professionals.
By using this website, you agree to our
Terms of Use,
Privacy Policy, and
Advertisement Policy.
For further details, please review our
Full Disclaimer.
Tags:
Recent News
Chennai: Fortis Healthcare Opens 250-Bedded 2nd Mu...
- 06 July, 2025
New Lab-On-A-Chip, Cheaper, Faster, On The Spot Di...
- 06 July, 2025
Steroids And Plasma Exchange Do Not Alter Prognosi...
- 14 February, 2020
Daily Newsletter
Get all the top stories from Blogs to keep track.


0 Comments
Post a comment
No comments yet. Be the first to comment!